
Introducing World Health Policy
Abstract
The COVID-19 pandemic has put an immense pressure on the world’s health systems and demonstrated the urgent need for a global health policy. This policy would allow world leaders to collaborate and respond quickly and effectively to not only the current COVID-19 crisis, but also future pandemics. Each country has its own unique health policies, which can be complex and difficult to navigate.
A deep understanding of health systems and healthcare systems is crucial in creating a solid foundation for standardized global health policy. By using a standardized approach, it would become easier to navigate the complexities of health policy and ensure that consistent terminology is used across the world. The creation of new standards for health policy is key to introducing a global health policy that is effective and efficient.
Moreover, a global health policy would ensure that countries are better equipped to respond to health emergencies in a coordinated and consistent manner. This would result in a more efficient use of resources and better outcomes for patients, regardless of where they are located in the world. With the ongoing threat of pandemics, a global health policy has become a necessity for ensuring the world is prepared for future health crises.
Introduction
The field of health policy is a complex and challenging one. This field continues to require the consideration of policymakers and those directly and indirectly impacted by established health policies. As such, health policy should be recognized as its own standalone discipline, one that requires regulation and standardization. This has already been demonstrated to be achievable in other areas of healthcare, such as health informatics and medical devices.
This paper focuses specifically on the difficulties posed by the ongoing COVID-19 pandemic and its impact on health policy in the United States and the European Union with regards to public health. The severity of the COVID-19 pandemic highlights the need for a unified international health policy. Such a policy would enable countries worldwide to coordinate their responses to not only the current COVID-19 crisis but also any future potential pandemics.
A healthcare system is a complex and multifaceted concept that has proven to be difficult to define. In the modern, complicated world, it might be difficult to give a precise definition of what a health system is, what it consists of, and where it starts and where it ends [1]. Busse [2] defined health system as an ”ensemble of all public and private organizations, institutions and resources mandated to improve, maintain or restore health. … encompass both personal and population services, as well as activities to influence the policies and actions of other sectors to address the social, environmental and economic determinants of health.”
A well-established global health policy would provide a shared understanding of best practices for responding to pandemics and access to shared resources and knowledge. This would facilitate coordinated efforts and effective allocation of resources, as all countries work towards a common goal. With the ongoing threat of pandemics, a comprehensive global health policy has become a necessity for ensuring the world is prepared for future health crises.
Health policy in Health System and Healthcare System
Healthcare system is defined by Medical Dictionary [3] as “Organized system of providers and services for health care; may include hospitals, clinics, home care, long-term care facilities, assisted living, physicians, health plans, and other services.” The term policy is not included in the definition of healthcare system. The definition of health systems includes the term policy (policies). Health policy is addressed through the health system rather than the healthcare system. Furthermore, healthcare systems and health systems can be used interchangeably [4]. White [4] defined health system based on World Health Organization (WHO) definition as “A health system comprises all organizations, institutions and resources whose primary intent is to improve health. In most countries, the health system is recognized to include public, private and informal sectors.”
Donev [1], Busse [2],Medical Dictionary [3], White [4], Mossialos et al. [5], Boulware et al. [6], Blumenthal et al. [7], Crowley et al. [8], Erickson et al.[9], Cancarevic et al. [10], Smokovski et al. [11] and Chang et al.[12] mentioned term ”system” without defining what this term means. Understanding the term system can help any reader to grasp the meaning of health system, healthcare system and health policy.The term system has various definitions depending on the field of its discipline. The closer definition to the term system used in health system is the definition introduced by Collin [13] as “a way of working, organizing, or doing something which follows a fixed plan or set of rules. You can use system to refer to an organization or institution that is organized in this way.”This definition is judged to be closer definition to health system because it contains organization and institution. Organization and/or institution are components of health system. Moreover, Sillitto et al. [14] looked at over 100 definitions of system in the attempt to understand perspectives, purpose and comprehend definition of the system. Sillitto et al. [14] understood that “system is a word, a label used to communicate a concept across people, so rather than being ascientific artefact, its most “correct”, “right”, or “best” definition can be judged by what allows for the most effective communication.” The effective communication means that people of certain discipline such as healthcare understand their roles and ensure that their work outputs are communicated and understood among the stakeholders in their system.
In order for a system to exist, the system must have a purpose and objectives to achieve. System constitutes of components and players to serve its stakeholders. The system’s purpose and objectives are governed by applicable laws and regulations. Both Donev [1] and Busse [2] definitions of healthcare system and health system have different purpose. The health system is the high level or parent system, and healthcare system is the child of the health system. The parent system encloses health policy. However, each healthcare system may have own health policy. In order to have a clear understanding and improve health policy in both healthcare system and health system, there is a strong need for standardisation of terminologies related to health policy. The standardisation has been proven to be possible in other healthcare fields such as health informatics. The standardisation may follow the process of ISO technical committee. The technical committee is therefore established to contain expert working group with representatives from different countries. The working group will create new standards for health policy.
Health policy in the EU and the US
According to Moutselos and Maglogiannis [15] health policy is referred by WHO as “decisions, plans, and actions that are undertaken to achieve specific health care goals within a society.” The US and the EU have different laws and different political thinking. Therefore, the US society and the EU society are influenced by different laws and different political decision making. The health policy in the US that govern the healthcare systems will not necessarily be fully similar to the EU health policy. Additionally, each EU member state has own health policies. Furthermore, each public hospital may have own health policy. Bulger et al. [16] suggested steps to guide policymakers on examining and evaluating the health policy. According to Bulger et al. [16], these steps were as follow: examine the public health interest, examine the overall effectiveness of the policy, evaluate whether the policy is well-targeted, identify the human rights burdens and examine whether the policy is the least restrictive alternative. Bulger et al. [16] suggested to have these elements in developing health policies: “impartial decision making, accountability, collecting full and objective information, applying well-considered criteria, and following a rigorous and fair process.”
Health policy is established by policymakers. Knowing or identifying these policymakers will help to understand how the health policy is established. According to Pressbooks [17] “policymaker is a synonym for ministry of health or whatever jurisdictional entity is responsible for the health of the population”. Policymakers, who are often accountable for the health of a certain population, are the ones who come up with ideas for new health policies. The responsible health policymakers in the US and the EU are required to adhere to the applicable laws and regulations in order to achieve the goal of ensuring that their citizens have access to high-quality medical care whenever and wherever it is necessary for them to receive it. The pandemic caused by COVID-19 has posed difficulties for health policy makers in both the US and the EU.
Impact of COVID-19 on the US and the EU health policies
The deadly virus COVID-19 took the EU and the US by surprise. The deficiencies of health policies in both the EU and the US were brought to light as a result of the COVID-19 pandemic. The virus has been spreading at an unprecedented rate, which led to the healthcare systems in these areas becoming overloaded. As a result, numerous hospitals have closed their doors. The effects of the pandemic were significantly more widespread and severe than the health authorities in the EU and the US had predicted or been prepared for. This underscores the necessity for rethinking and reengineering of these policies in order to better prepare for pandemics in the future.
Moutselos and Maglogiannis [15] stated that “policymaking must be based on scientific evidence”, this is true, but it is not enough. Humphreys and Piot [18] recognized that “scientific evidence alone is not sufficient basis for health policy”. Scientific evidence may be jeopardized by political decision-making. The COVID-19 requires one global health policy where scientific evidence and political decision-making are aligned to save lives and boost the economic growth around the globe. The COVID-19 pandemic has shown that collaboration between scientific evidence and political decision-making are required in order to effectively address global health emergencies. This was proved by the pandemic. It would be desirable to have a global health policy that, under the auspices of the United Nations (UN), works in conjunction with the World Health Organization (WHO), and brings together the health policymakers and health experts from around the world. This would ensure that the scientific data is heard and presented to the public, as well as that political collaboration exists among the leaders of health ministry organizations to combat the epidemic.
In spite of the efforts of health authorities, a significant number of the populations of both the EU and the US continue to harbor reservations over the administration of the COVID-19 vaccination. The proliferation of false information across social media platforms is one factor that contributes to this pessimism, which in turn contributes to mistrust in governmental health organizations. The UN and the WHO need to collaborate on the development of a solid world health policy that the general public can have faith in. This policy should emphasize the significance of early containment of the virus in contaminated areas and be based on the lessons learnt from the current epidemic. It should also get full support from all world governments. The WHO is able to successfully organize the policy’s execution and respond to the needs of both present and future pandemics because it has developed a global health policy.
Health system performance and standardization of health policy
According to Nolte and Merkur [19] assessing the performance of the health system is assessed on micro, meso and macro level. The micro level focuses on assessing the process of patient care. The micro level is assessed through the comparison of teams that deliver patient care. The meso level focuses on assessing organizational context. This level is assessed by comparing organizations (i.e., hospitals) performance. The macro level focuses on assessing financing and policy context. By looking at the micro, meso and macro levels, I see that the policy is addressed on macro level. Furthermore, Nolte and Merkur [19] informed that the performance under the macro policy aim to monitor, evaluate and communicate the extent to which various aspects of health system meet their objectives. The health policy must ensure that patients get the appropriate health services that meet their health outcome expectations. The performance from health outcome perspective is beneficial if it meets the quality that is expected by patients.
Based on Moutselos & Maglogiannis [15], Bulger et al. [16] and Nolte & Merkur [19], the adoption of the ISO 13485:2016 [20] quality policy can serve as a ground for quality health policy where top management of any health care organization shall ensure that the quality health policy:
a) is applicable to the purpose of the health care organization.
b) includes a commitment to comply with requirements and to maintain the effectiveness of the healthcare system
c) provides a framework for establishing and reviewing health care objectives
d) ensure that quality health policy is communicated and understood within the health care organization
e) health policy is reviewed for continuing suitability of the health organization
Additionally, top management shall ensure that quality health policy objectives are established at relevant functions and levels within the health care organization. The health care organization objectives shall be measurable and consistent with the health policy. The proposed quality health policy will be beneficial if it will cover all aspects of micro, meso and macro levels of any health organization. The quality health policy standardization will help to build foundation for global health policy.
Proposed framework for global health policy
Table 1 shows a proposed framework for establishing global health policy. Other health policy researchers will be required to continuously improve this framework. The proposed health policy framework is being improved with input from UN political leaders and WHO health policy experts with international experience in the field of health systems. It is strongly advised to form a global health policy expert panel. This panel will include experts from each of the UN member countries. The goal is not to reinvent the wheel, or to coin new terms for global health policy. The proposed framework employs terminology similar to micro, meso, and macro levels. The use of existing terminology will make standardizing global health policy easier.
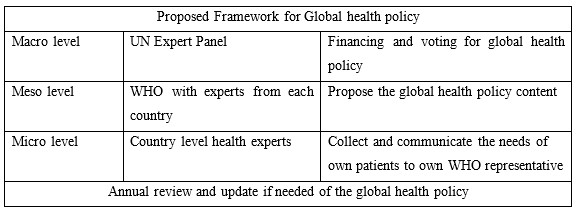
Table 1: Proposed framework for global health policy
The UN expert representatives will be in charge of funding and voting on proposed health policies at the macro level. Globally, the UN will ensure political engagement and awareness of current and future health issues. The global health policy will allow world leaders to coordinate their efforts. The coordination will allow world leaders to act in a timely manner to contain any virus spread before it becomes a pandemic concern. Global health policy is required to develop action plans for the current pandemic and to be prepared for any future global health challenges. The UN leaders will secure funding to address global health challenges.
The global health policy content is discussed at the meso level. It is recommended to have experts from each country discuss the global health policy content at WHO.
The micro level is the country level, where policymakers and relevant health experts gather and communicate the needs of their own patients to their own WHO health expert representative.
Conclusion
It is strongly advised that health policy experts (academic, political, and clinical experts) introduce new ISO standards in order to have a well-defined policy in the health system or healthcare system. A system that can be audited and evolved to identify healthcare barriers and contribute to health quality improvement. The new ISO health policy standard will aid in the development of a framework for utilizing healthcare services efficiently. Furthermore, the standard will be designed in such a way to help governments all over the world to be resilient and ready for any future pandemic. The standards will enable health policy experts to communicate in a common language, facilitating global health policy.
References
[1] Donev, D., Kovacic, L. and Laaser, U., 2004. The role and organization of health care system. Health system and their evidence based development. Lage: Hans Jacobs Publishing Company, pp.19-46.
[2] Busse.R. 2014. Busse, R. The contribution of health systems research to HSR: time to know what we are talking about, and why it is important for evidence-based policy-making. BMC Health Serv Res 14 (Suppl 2), O25. https://doi.org/10.1186/1472-6963-14-S2-O25.
[3] Medical Dictionary. Health care system. Available at:
https://medical-dictionary.thefreedictionary.com/health+care+system (Accessed on 02.02.2021).
[4] White, F., 2015. Primary health care and public health: foundations of universal health systems. Medical Principles and Practice, 24(2), pp.103-116.
[5] Mossialos, E., Wenzl, M., Osborn, R. and Sarnak, D., 2016. 2015 international profiles of health care systems. Canadian Agency for Drugs and Technologies in Health.
[6] Boulware, L.E., Cooper, L.A., Ratner, L.E., LaVeist, T.A. and Powe, N.R., 2016. Race and trust in the health care system. Public health reports.
[7] Blumenthal, D., Fowler, E.J., Abrams, M. and Collins, S.R., 2020. Covid-19—implications for the health care system.
[8] Crowley, R., Daniel, H., Cooney, T.G. and Engel, L.S., 2020. Envisioning a better US health care system for all: coverage and cost of care. Annals of internal medicine, 172(2_Supplement), pp.S7-S32.
[9] Erickson, S., Outland, B., Joy, S., Rockwern, B., Serchen, J., Mire, R.D. and Goldman, J.M., 2020. Envisioning a better US health care system for all: health care delivery and payment system reforms. Annals of internal medicine, 172(2_Supplement), pp.S33-S49.
[10] Cancarevic, I., Plichtová, L. and Malik, B.H., 2021. Healthcare Systems Around the World. In International Medical Graduates in the United States (pp. 45-79). Springer, Cham.
[11] Smokovski, I., 2021. Benefits of Centralized e-Health System in Diabetes Care. In Managing Diabetes in Low Income Countries (pp. 73-83). Springer, Cham.
[12] Chang, A., Cullen, M.R., Harrington, R.A. and Barry, M., 2021. The impact of novel coronavirus COVID‐19 on noncommunicable disease patients and health systems: a review. Journal of internal medicine, 289(4), pp.450-462.
[13] Collin. Definition of ’system’. Available at: https://www.collinsdictionary.com/dictionary/english/system (accessed on 20 May 2021).
[14] Sillitto, H., Dori, D., Griego, R.M., Jackson, S., Krob, D., Godfrey, P., Arnold, E., Martin, J. and McKinney, D., 2017, July. Defining “system”: A comprehensive approach. In INCOSE International Symposium (Vol. 27, No. 1, pp. 170-186).
[15] Moutselos, K., Maglogiannis, I., 2020. Evidence-based Public Health Policy Models Development and Evaluation using Big Data Analytics and Web Technologies. Medical Archives, 74(1), p.47.
[16] Bulger, R.E., Bobby, E.M. and Fineberg, H.V., 1995. The Formulation of Health Policy by the Three Branches of Government. In Society’s Choices: Social and Ethical Decision Making in Biomedicine. National Academies Press (US).
[17] Pressbook. 2021. INTRODUCING THE KEY STAKEHOLDERS: PATIENTS, PROVIDERS, PAYORS, AND POLICYMAKERS (THE FOUR P’S). Available at: https://jln1.pressbooks.com/chapter/3-introducing-the-key-stakeholders-patients-providers-payors-and-policymakers-the-four-ps/ (accessed 14.05.2021).
[18] Humphreys, K. and Piot, P., 2012. Scientific evidence alone is not sufficient basis for health policy. Bmj, 344.
[19] Nolte, E. and Merkur, S., 2020. Achieving Person-Centred Health Systems. Cambridge University Press.
[20] ISO 13485:2016 Medical devices – Quality management systems – Requirements for regulatory purposes.